I never imagined I would be writing a post like this—one that forces me to lay out in stark terms a diagnosis that has rocked my world in ways I’m still trying to process. But here I am, ready to talk about what’s been going on with my health, what I’ve learned so far, and how I’m trying to navigate the journey ahead. I have Adhesive Arachnoiditis, a rare and progressive spinal disease. While I’m no fan of dramatics or doom-and-gloom pronouncements, some doctors do speculate that the lifespan of someone with Adhesive Arachnoiditis can be in the range of four to ten years. That’s a chilling number, and one I’m still trying to wrap my head around.
Yet, I want to be straight with you: I won’t be sugar-coating anything here. I also don’t plan on placing absolute stock in what any single doctor says—because, let’s face it, the medical community doesn’t always agree, and every individual’s situation is different.
Understanding Arachnoiditis
Before I dive into how I’m handling this emotionally, let me shed some light on what Arachnoiditis actually is. It’s an inflammation of the arachnoid lining of the spinal cord. The arachnoid is one of the membranes that surround and protect the spinal cord and nerves. When it gets inflamed—often due to things like infections, spinal surgeries, or other direct trauma to the spine—it can lead to chronic pain, neurological problems, and a progressive degeneration of the nerves in the spinal column. In other words, it’s bad news.
The hallmark symptom is severe, relentless pain. That’s the part doctors and patients talk about the most, but it doesn’t stop there. Some people experience numbness, tingling, muscle cramps, or, ironically, both numbness and searing pain in the same limb. It’s a strange, unpredictable condition. In my case, I have a combination of chronic pain that pulses down my back and through my legs, sometimes paired with sudden twinges of numbness that seem to pop up out of nowhere.
One big misconception is that if you “just” have chronic pain, you can push through it. Take a couple of painkillers, use a heating pad, get some massages—poof, you’ll manage. But Arachnoiditis doesn’t work that way. It’s not just a pulled muscle or a slipped disc that can be eased with some physical therapy and an epidural injection. The entire structure of the nerves can become compromised, meaning permanent damage that doesn’t always respond to conventional treatment. This is where skepticism about the disease sets in for a lot of people, including some medical professionals who might not realize just how debilitating it can be.
Early Signs and the Diagnosis Journey
Like many chronic illnesses, my path to a diagnosis was anything but straightforward. I first noticed sporadic back pain a few years ago. Everyone gets backaches from time to time—especially if you spend hours in a desk chair or do any kind of physical labor—so I shrugged it off. Then, the pain started to intensify. Sometimes I’d feel a dull ache that just wouldn’t go away; other times it felt like electric shocks running down my legs. Occasionally, I had trouble walking straight, or even standing up for extended periods.
Initially, I was diagnosed with a “simple” herniated disc. I went through months of physical therapy. But as months turned to years, the pain didn’t get better. In fact, it got worse, like a flame slowly building into a relentless fire. My primary care doctor FINALLY ordered an MRI, and they found a tumor in my spinal cord.
In 2023, I spent 10 days in the hospital, where they removed the thankfully benign Schwannoma tumor. I thought I’d get back to normal after several months and that my prognosis was good. I was sadly mistaken.
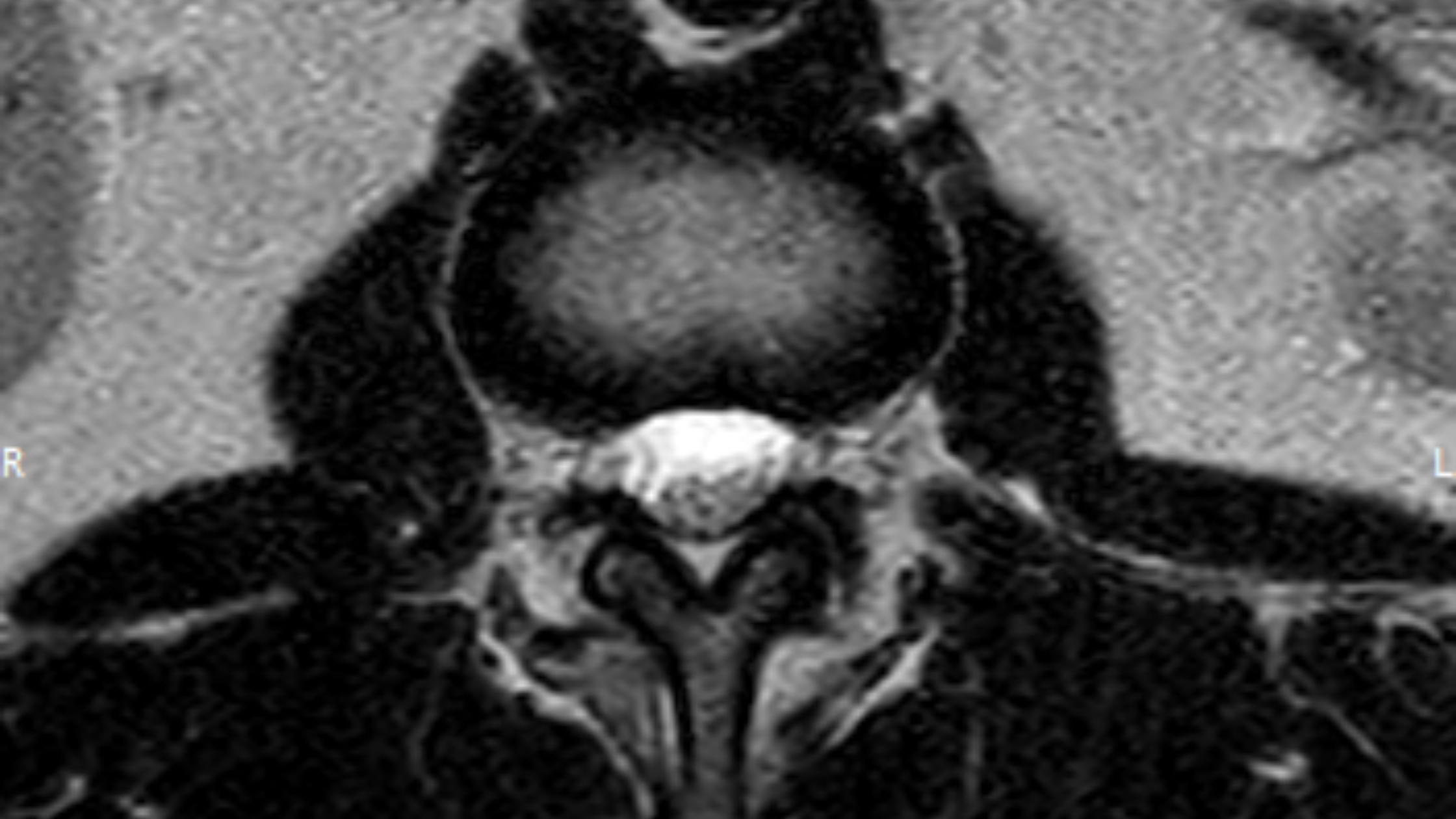
I started noticing new symptoms along the way—random muscle cramps, numbness along my right side from my waist down, and burning sensations shooting down my legs when I stood or walked for too long. A new MRI in November of 2024 finally revealed signs of Arachnoiditis: the nerves in my spinal canal were clumping together, and the membrane was inflamed. The spinal doctor who pointed it out spoke in a grave tone, one that suggested a major shift in my world. He was direct: “This is going to change your life.” His words have echoed in my mind ever since.
Processing the “4-10 Year” Lifespan Speculation
Let me address the elephant in the room: some doctors say that individuals with Adhesive Arachnoiditis might only live four to ten years after diagnosis, especially if the condition causes severe complications or accelerates rapidly. Hearing that range was like taking a punch to the gut. I’m skeptical by nature, so I’m not taking it as an absolute. Life expectancy forecasts can be all over the place. Medical opinions evolve, and plenty of people defy those odds and live longer—sometimes much longer.
Still, it’s impossible not to feel a surge of fear and existential dread. I keep catching myself thinking, “If I only have a decade or less, how do I make the most of it?” That might be a cliché question, but it’s a question I now face with genuine urgency. On my good days, I’m optimistic that treatment advances or just plain luck will keep me around for longer. On my bad days, I’m overwhelmed by the possibility that time is short, and that I might need to start making tough decisions about my future right now.
Why I’m Writing This Blog Post
I debated whether or not to go public. It’s hard enough to talk about something this severe with my closest friends and family, let alone the entire internet. But eventually, I realized that writing has always been my way of processing the unprocessable. It’s my lifeline for clarity, for emotional release, and for bridging the gap between my experiences and other people’s understanding.
So this post serves a few purposes:
- Informing those who care: Instead of having to explain the diagnosis in one-off conversations that leave me emotionally drained each time, I’m using this platform to share in one broad stroke.
- Raising awareness: Arachnoiditis isn’t a household name. If I can help even one other person recognize the symptoms, or one doctor to consider this diagnosis in a patient, then I’ve done some good.
- Self-preservation: I’m trying to own my narrative here. Sharing my struggle in my own words is a way to feel a semblance of control in a situation that is inherently uncontrollable.
Living with Chronic Pain: No Easy Fixes
Chronic pain is isolating. It seeps into every corner of your life, restricting your mobility, your comfort, your social interactions. It can also fuel anxiety and depression because you constantly have to strategize about how you’ll manage the pain on any given day. Will I be able to drive without my back spasming? Will standing in line at the grocery store be too much for me this week? This disease hijacks your decision-making process, making every action contingent on pain management strategies.
I’ve learned the importance of pacing—of not pushing myself too hard on good days because that can lead to disastrous flare-ups that put me in bed for a week. I’ve grown to appreciate small things like quiet mornings when my body isn’t screaming at me, or the times I can still go for a hike without feeling like I’m running a gauntlet.
It’s easy to feel demoralized, especially when people around you might downplay what you’re going through. “You look fine,” they say. “Have you tried yoga?” or “You just need to move more.” The unsolicited advice never ends. It’s as if the severity of the illness is invisible, and, to be fair, that’s the crux of conditions like these: they’re silent but crushing, invisible but life-altering.
Navigating Medical Opinions and Misinformation
One of the most frustrating aspects of dealing with Arachnoiditis is the patchwork of conflicting opinions. Some doctors are up to speed on recent literature and empathize with your struggle. Others have never treated a single case and might downplay your symptoms. Then there’s the online information that ranges from outright misinformation—miracle cures and conspiracies—to legitimate research scattered across obscure medical journals.
I’m in a place now where I’m trying to gather information from multiple sources. I see specialists, read up on newly published studies, and listen to patient stories in online communities. I don’t take any single viewpoint as gospel. A healthy dose of skepticism is warranted when your life may literally depend on the quality of information you receive. And that’s part of why I’m sharing this: I want to point out that if you’ve been handed a tough diagnosis—whatever it is—never stop questioning, investigating, and taking an active role in your own healthcare.
Treatment Options: Hope vs. Reality
There’s no magic bullet for Arachnoiditis, at least not yet. Existing treatment focuses on symptom management:
- Medication: Painkillers, muscle relaxants, and sometimes off-label prescriptions that target nerve pain. They can help to some degree, but come with side effects like drowsiness, digestive problems, or dependency issues.
- Physical Therapy: Carefully curated exercises can maintain flexibility and mobility, but they don’t always stop the pain. Overdoing physical therapy can trigger extreme flare-ups.
- Steroid Injections: Ironically, steroid injections themselves can sometimes cause or worsen Arachnoiditis in certain circumstances, which is a terrifying possibility. So that’s a catch-22.
- Surgery: Some surgeons might attempt to remove scar tissue or decompress nerves, but surgery also carries the risk of further nerve damage. For Arachnoiditis patients, surgery might bring fleeting relief or could make things worse.
- Alternative Approaches: Acupuncture, mindfulness, nutritional adjustments, or even experimental procedures. Results can vary, and it’s hard to separate placebo effect from real progress.
If you sense a skeptical tone here, it’s because I’ve seen how often these treatments fall short or only provide temporary relief. That said, I’m not giving up on the hope that something might work for me. It might take a combination of these treatments—or something entirely new. Medical research is always ongoing; new therapies could emerge in the coming years that shift the outlook dramatically.
Mental and Emotional Resilience
Coming to terms with a serious diagnosis is as much a psychological battle as it is a physical one. There are days I wake up feeling shattered by the weight of it all—the relentless pain and the uncertain horizon. On those days, despair is more than a passing emotion; it’s a state of being.
I’m learning to accept that it’s okay to have days like that. I’m not aiming for relentless positivity. But I also don’t want to be swallowed by hopelessness. This is where I’m trying to lean on my support system—family, friends, counselors, online communities of fellow chronic illness warriors. Even just a phone call or text from someone who acknowledges my pain helps me feel less alone in it.
I’m also learning that self-compassion is non-negotiable. It’s easy to beat yourself up for not being able to do what you used to do or for “inconveniencing” other people with your needs. But the reality is that you can’t will away a progressive disease. No amount of “positive thinking” alone is going to rebuild frayed nerves. So I’m trying to find balance between honesty about my limitations and maintaining a drive to keep going as best I can.
Facing the Unknown Future
Let’s talk about that 4-10 year possibility. It’s a frightening concept. Does it mean I should rush out and complete a bucket list? Should I try to maintain life as usual until something forces me to stop? Or do I seek out every experimental therapy known to humankind? The truth is, I don’t know. And I suspect many people who get a serious prognosis feel similarly lost at first.
What I do know is that hearing a timeframe has forced me to confront what matters most. I’m prioritizing relationships, experiences, and creative pursuits that feed my soul. I’m cutting back on unnecessary stressors that tend to sap my energy. This diagnosis is like a rude awakening that pushes you to clarify your values in record time.
I’m also not entirely convinced that 4-10 years is etched in stone. Everyone’s body is different, and “average” prognoses leave out the variability of individual stories. I could deteriorate faster than expected, or I could outlive that prediction by a wide margin. And until the day comes when we have definitive answers, I’m keeping a mixture of realism and hope in the forefront of my mind.
What I Ask of You
If you’re reading this because you know me personally, I have a couple of requests:
- Patience: This condition might force me to cancel plans last-minute or withdraw socially when the pain is intolerable. I appreciate every bit of understanding you can muster.
- No Pity Parties: Empathy is wonderful, but please don’t treat me like a lost cause. I’m still very much here, still craving connection, laughter, and meaning.
- Curiosity: If you haven’t heard of Arachnoiditis before, spend a little time reading up on it. Knowledge fosters empathy, and you could help spread awareness.
Looking Forward: Skeptical, Yet Hopeful
I’d be lying if I said I’m 100% confident I’ll beat the odds. Then again, I’m not rolling over and surrendering, either. There’s too much I still want to do, too many stories left to write, and too many sunsets left to watch.
The medical field evolves quickly, and even if the odds are against me, it’s in my nature to question them. I’m still exploring different treatment avenues, still seeking answers from specialists. I’m also trying to live a life that honors my values—connecting with loved ones, writing from the heart, and not letting fear dictate every choice I make.
Some days that’s easier said than done. It’s a balancing act—being realistic about pain and physical limitations while stubbornly refusing to give up on the joys life has to offer. That’s the path I’m walking now, and this blog post is just one step on that path.
Closing Thoughts
I don’t have a neat, uplifting conclusion to tie this all together because life with a progressive condition seldom wraps up with a bow. But I will say this: this diagnosis is part of who I am now, not the sum total of my identity. I can be honest about how dark things can get without losing sight of the light that’s still out there.
For those of you who are here to support me, thank you. For those who are in a similar boat, I see you—and I hope this post brings you some sense of solidarity. Arachnoiditis may be a tough opponent, and the speculation around life expectancy can feel like a looming shadow, but I’m not willing to let that define the time I have left—whether it’s four years, ten years, or far beyond.
Thanks for reading, for caring, and for joining me in pushing forward with open eyes, clear minds, and a healthy dose of skepticism about what the future may hold. It’s not going to be easy, but if nothing else, I’m determined not to let a bleak prognosis rob me of the time I do have. I’ll continue to question, to seek new paths, and to share updates here when I can. Life is precious, no matter how long it lasts, and while I might be staring down some tough odds, I still plan on making every moment I can truly count.
Disclaimer: This blog post reflects my personal experience and is not intended as medical advice. Always consult with a healthcare professional before making any changes to your treatment plan.
8 Responses
We, as grandparents, are so proud of your post and will follow each one as you travel through this journey.
Jason- thanks for sharing in a way that helps us understand. This has shaken us all to the core. You are right, it has a way of creeping up on all of us and was difficult to comprehend. What I do know is the I love you and many people love you. We care about you. We want to do what we can to explore solutions, to give comfort and to be here for you. You are not alone. I am glad you shared this.
Love your Dad, Lucy , Joanna and Tommy.
Such a phenomenal post. I am so proud of you and will be supporting you through it all. Wishing you all love.
It is not an easy diagnosis to deal with for sure but we are here to help you and support you . We are still exploring options and trying to find solutions . If there is a treatment in the world we will find it. We want you around for a long time and we do not quit easy. Doctors are wrong sometimes and miracles happen too. Please keep thinking positive and know that you always can depend on us and please feel free to ask for help if needed. You are not alone in this battle . Please, remember that . There are lot of people that care about you
Jason – .I am a colleague ( I’m a healthcare executive ) and friend of your father Jeff. I know he has started and will continue to search for solutions to help with your journey. He and I have a vast network of healthcare professionals we can reach out to for information. Hang tight and stay strong your father is one in a million and can find a diamond in a bail of hay.
Eloquent, reasonable, rational, and inspirational – thank you for sharing. Your family and friends certainly want to know how you are doing – but not at the expense of leaving you crushed emotionally with each explanation and update.
We are here for you and will do anything possible to support you and your family as you continue this journey. Finding the “new normal” may include some last minute adjustments to best support you (as your path may not be linear) – and you will certainly have our understanding and full support in making whatever adjustments are needed.
Please keep up the research, skepticism, hard work, and writing – I’m glad you find it therapeutic.
Jason, we love you. Thank you for helping us all to understand better not just what’s going on but also how it affects you emotionally.
PLEASE do not hesitate to call and let us know – and do – anything we can to help you, Lee, or the boys.
Jason,
I am your comrade. I have no idea how I stumbled upon your blog, but it was God sent. I was diagnosed last June, a week after my Mom passed away w an excruciating battle with lung cancer. I was in shock. You described hearing “those” words ( as we all hear different but same ones ) so perfectly. I had surgery for L4,L5 and was told if I didn’t repair them I’d be paralyzed waist down. Imagine walking in and hearing that ?
Well of course the surgery recovery has not gone as planned. I woke up with a neurongenic bladder and bowels, pereneal anesthesia ( no feeling) and my left leg was 75% numb , right about 50. I have no feeling in my toes and can’t straighten my foot.
I had NONE of this prior to surgery and had very little if any symptoms of my AA. A patch of numb skin near my buttocks, that I assumed was from one of my MANY epidurals ( that I had ABSOLUTELY no idea could cause this )
I was told it was normal and would go away in “time” Fast forward almost 9 months. I have progressed surgery wise ( can walk and shower , difficulty w stairs etc ) but the conditions I woke to are exactly the same. So I find myself now having to take a hard look at arachnoiditis ( the thing I could put away while life was happening HARD at me ) I found YOUR article that I now can share with family and friends when I am explaining AA rather than “google” 🤣.
I could have written this myself
Thank You for representing “us”
The support groups IMHO are anything but… they make me MORE depressed and sad. There very little offerings of things that have helped. My heart breaks for these people, I just have preserve my well being right now and can’t be their support, if you know what I mean. I am that “one” who will be one there taking everyone’s pain.
So now I’m trying to EVEN FIND a doctor who knows anything about it . THE MOST FRUSTRATING PART SO FAR. I am inthe Boston area w the top hospitals and doctors in the world. Like finding a needle in a haystack. My three month wait to get into a pain clinic was for naughty as no one had ever dealt with it, they primarily give epidural shots 🙄😡.
So from the bottom of my heart I thank you. If you ever want to reach out to me if you do find anything my email is gobrien624@gmail.com.
I will keep you and your family ( you have a wonderful supportive family, blessed to have so many rooting and researching for you )I know the toll it takes on loved ones powerless to help day in and day out. All of them and you are in my prayers for Peaxe and Strength as we try and continue to live with the “new normal “ . It’s not the one we thought we’d have but it’s the one we’ve got so let’s make the best of each day, one at a time
😘🙏🏻🙌🏻💕💞😇