Living with adhesive arachnoiditis has been an arduous journey, marked by relentless pain, uncertainty, and a continuous battle against inflammation. In this post, I want to share my personal story, delve into the science behind inflammation and its profound impact on adhesive arachnoiditis, and explain how I’m taking control of my health with a groundbreaking tool: the COR One device from COR Health (www.corhealth.com). With this device, I will track my body’s inflammation on a weekly basis by monitoring my Erythrocyte Sedimentation Rate (ESR), a marker that captures a wide array of inflammatory pathways.
Understanding Adhesive Arachnoiditis
Adhesive arachnoiditis is a rare yet devastating condition affecting the arachnoid, one of the thin membranes that envelop the spinal cord. Normally, the arachnoid serves as both a cushion and a protective barrier, but in this condition, inflammation ignites a cascade of events that result in the formation of scar tissue and adhesions. These adhesions can bind nerve roots together, leading to chronic pain, neurological deficits, and a myriad of other symptoms that severely compromise quality of life.
The onset of adhesive arachnoiditis can follow various triggers such as spinal surgery, trauma, infections, or even procedures like epidural injections. Once the inflammatory process begins, the body’s healing mechanisms go into overdrive. Instead of healing in a regulated fashion, the body produces excessive scar tissue. Over time, these adhesions can exacerbate pain by continually irritating nerve fibers, resulting in a vicious cycle of inflammation and tissue damage.
The Role of Inflammation in Adhesive Arachnoiditis
Inflammation is the body’s natural response to injury or infection. In its acute form, inflammation is beneficial—it isolates harmful agents and initiates tissue repair. However, when inflammation turns chronic, it becomes a double-edged sword. In adhesive arachnoiditis, chronic inflammation is not only a symptom but also a driving force behind the condition.
Chronic inflammation leads to the persistent activation of the immune system, resulting in the release of various inflammatory mediators such as cytokines and prostaglandins. These substances, while essential in the healing process, also contribute to the formation of scar tissue and adhesions when their production goes unchecked. As inflammation continues, it inflicts further damage on tissues, perpetuating a cycle that intensifies nerve entrapment and exacerbates pain.
Understanding the complex role of inflammation is critical when it comes to managing adhesive arachnoiditis. By identifying and targeting the triggers of chronic inflammation, there is hope to break this cycle, reduce pain, and potentially limit the progression of scarring. This quest for control over inflammation is at the heart of my personal health experiment.
Inflammation: The Good, The Bad, and The Chronic
It is important to recognize that inflammation in itself is not inherently negative. In its acute phase, inflammation is indispensable for healing. For instance, when you sustain a minor injury, the immediate inflammatory response helps to fend off infections and begin tissue repair. The problem arises when inflammation lingers long after the initial injury—a state known as chronic inflammation.
Chronic inflammation is a stealthy adversary. It can persist for months or even years without dramatic symptoms, slowly inflicting cumulative damage on the body. In the context of adhesive arachnoiditis, this persistent inflammation initiates and perpetuates a harmful cycle: injury leads to inflammation, which in turn causes further tissue damage, inviting more inflammation. Interrupting this loop is a primary target of many modern therapeutic strategies, which include anti-inflammatory medications, physical therapy, and lifestyle interventions like improved diet and stress management.
Given the central role of inflammation in adhesive arachnoiditis, I began exploring ways to monitor my body’s inflammatory state more precisely. This exploration eventually led me to a promising technological solution.
Introducing the COR One Device from COR Health
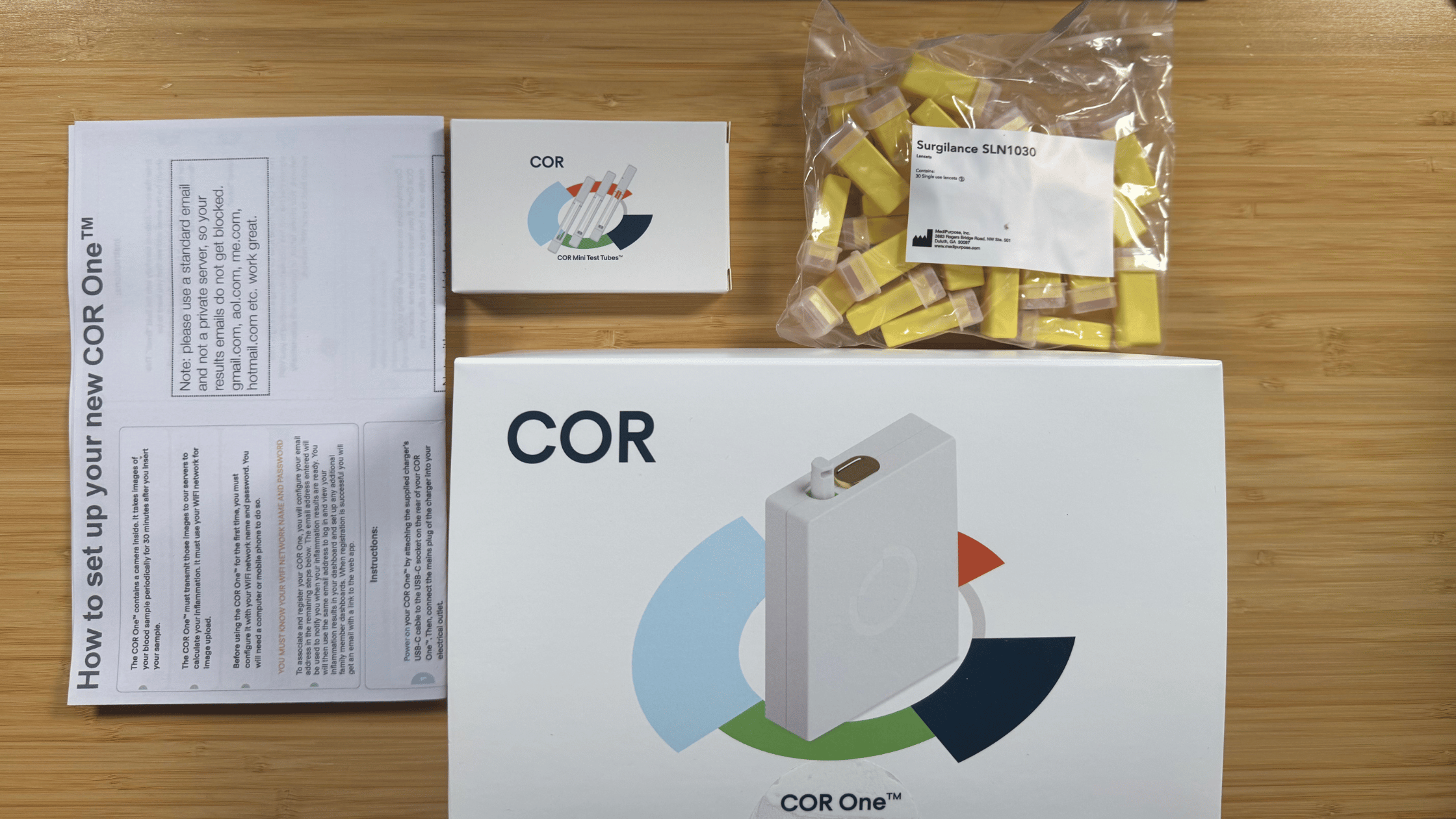
Today, I received the COR One device from COR Health. Unlike conventional methods of assessing inflammation, which often rely on infrequent and invasive blood tests to measure markers like C-reactive protein (CRP), the COR One device offers a unique and non-invasive approach. It specifically tracks the Erythrocyte Sedimentation Rate (ESR), a critical marker that reflects the overall inflammatory state of the body.
ESR is a well-established indicator used in clinical settings to assess inflammation. It measures how quickly red blood cells settle at the bottom of a test tube over a specified period. The rate at which they settle is influenced by the presence of proteins and other factors in the blood that are elevated during inflammatory states. By tracking ESR, the COR One device provides a comprehensive snapshot of systemic inflammation, capturing a broader spectrum of inflammatory pathways than many other markers.
This focus on ESR is particularly valuable because it not only gives insights into the acute phase of inflammation but also detects more subtle, chronic changes. For someone managing a condition as complex as adhesive arachnoiditis, this level of detailed, objective data is a game changer.
My Experiment: Weekly Inflammation Monitoring with ESR
Adopting a proactive approach to health management, I plan to integrate the COR One device into my weekly routine to track changes in my inflammation levels via ESR. Here’s how I’m planning to use this innovative tool and what I hope to learn from the experiment:
Establishing a Baseline
The first step in any self-experiment is to establish a reliable baseline. For several weeks, I will use the COR One device to record my ESR levels without making significant changes to my lifestyle or treatment regimen. This baseline will serve as a reference point against which I can compare future data. Understanding my natural inflammatory state will allow me to discern the effects of any interventions I implement later.
Testing Different Interventions
After I have a stable baseline, I will introduce various interventions one at a time to see how they influence my ESR and, by extension, my overall inflammatory status. Some of the interventions I’m considering include:
- Dietary Adjustments: I plan to experiment with an anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and whole, nutrient-dense foods. Concurrently, I will avoid processed foods, sugars, and trans fats. By correlating my weekly ESR readings with dietary changes, I aim to determine if these modifications lead to a measurable decrease in inflammation.
- Exercise Regimens: Exercise is a known modulator of inflammation, yet its effects can vary greatly among individuals with chronic pain. I will experiment with different types and intensities of exercise—from stretching routines to moderate cardiovascular workouts and weight training—to identify what best supports my body without triggering excess inflammation.
- Stress Management Techniques: Chronic stress is a significant contributor to systemic inflammation. I will incorporate stress-reduction strategies such as meditation, mindfulness exercises, and breathing techniques into my routine. By monitoring how these practices influence my ESR, I hope to see a direct correlation between reduced stress and lower inflammation levels.
- Improving Sleep Quality: Sleep is essential for recovery and the regulation of inflammatory responses. I plan to assess how changes in my sleep patterns affect my ESR readings. Ensuring adequate and restful sleep might be a key factor in controlling my chronic inflammation.
- Medication and Supplementation: I intend to monitor any adjustments to medications or supplements to see how these changes impact my ESR levels, using the COR One device as an objective measure to fine-tune my treatment strategy.
Analyzing the Data and Personal Insights
One of the most exciting aspects of this experiment is the opportunity to generate personalized, actionable data. I will maintain a detailed log of my ESR readings alongside records of any lifestyle changes, dietary modifications, exercise routines, and stress management techniques. By analyzing this data over time—using graphs and trend lines—I hope to uncover clear patterns that reveal which interventions effectively reduce inflammation.
This personalized approach empowers me to make informed decisions about my health. Rather than relying solely on anecdotal evidence or general guidelines, I will have objective data that tells me how my body reacts to specific changes. This data-driven method is not only empowering but also a promising step toward managing adhesive arachnoiditis more effectively.
The Broader Implications of ESR Monitoring
The COR One device’s focus on ESR offers a unique advantage in understanding and managing chronic inflammatory conditions. ESR is sensitive to a wide range of inflammatory signals, making it a robust marker for capturing the complexities of systemic inflammation. This can be particularly valuable for conditions like adhesive arachnoiditis, where inflammation is both a symptom and a contributing factor to disease progression.
Why ESR?
- Comprehensive Inflammatory Insights: Unlike some markers that may only provide a snapshot of acute inflammation, ESR reflects changes across multiple inflammatory pathways. This makes it a more comprehensive indicator of the body’s overall inflammatory status.
- Non-Invasive and Convenient: The ability to track ESR on a weekly basis using a non-invasive device like the COR One allows for continuous monitoring without the discomfort or inconvenience of regular blood draws. This continuous feedback loop is essential for understanding the dynamic nature of chronic inflammation.
- Tailored Interventions: With detailed ESR data, I can tailor my interventions more precisely. Whether it’s adjusting my diet, modifying my exercise routine, or experimenting with new stress-relief techniques, I will be guided by objective data that reflects my body’s response to these changes.
Looking Forward: A Data-Driven Path to Better Health
Embarking on this journey of self-monitoring and data-driven experimentation is both exhilarating and empowering. Adhesive arachnoiditis has long been a condition that feels uncontrollable due to its chronic inflammation and unpredictable flare-ups. However, with the COR One device at my side, I have a new tool that offers insight, guidance, and hope.
Unraveling the Inflammation Puzzle
I am determined to decipher the complex interplay between lifestyle factors and inflammation. By tracking ESR weekly, I hope to identify specific triggers—whether they be dietary, physical, or emotional—that consistently lead to spikes in my inflammatory markers. This knowledge will be critical in crafting a personalized strategy to manage my condition more effectively.
Empowering Personalized Healthcare
The future of healthcare lies in personalization. Each of us responds differently to interventions, and understanding these nuances is key to effective treatment. My experiment with the COR One device is a step toward personalized healthcare, where my treatment is guided not by general protocols but by the unique signals my body sends through ESR. This approach has the potential to improve not just my quality of life, but also contribute to a broader understanding of chronic inflammatory conditions like adhesive arachnoiditis.
Contributing to the Broader Conversation
Adhesive arachnoiditis remains a condition that is not widely understood, even within the medical community. By sharing my journey and the data I collect, I hope to spark a broader conversation about the role of inflammation in chronic pain conditions. My experiences—and the insights gleaned from continuous ESR monitoring—may offer valuable lessons for others grappling with similar health challenges. Each data point is a small piece of the larger puzzle that, collectively, could lead to more effective management strategies for chronic inflammation.
A Look Ahead
As I step into this new chapter of self-discovery, I remain cautiously optimistic about the road ahead. There is no denying that managing adhesive arachnoiditis is a formidable challenge. Yet, by harnessing advanced technology and adopting a proactive, data-driven approach, I am hopeful that I can regain some control over my body’s inflammatory responses.
I invite you to join me on this journey. In the coming weeks and months, I will be sharing regular updates, insights, and lessons learned from my weekly ESR monitoring. Whether you are dealing with a similar condition, fascinated by the science of inflammation, or simply interested in the potential of personalized healthcare, I hope you find my experiences both informative and inspiring.
In a world where chronic conditions often leave us feeling powerless, tools like the COR One device represent a beacon of hope—a way to transform subjective symptoms into objective data that empowers us to make informed decisions about our health. Here’s to taking control of our well-being, one week at a time, and to the promise of a future where personalized healthcare leads us toward a better quality of life.
Disclaimer: This blog post reflects my personal experience and is not intended as medical advice. Always consult with a healthcare professional before making any changes to your treatment plan.
One Response
Wow. So impressive. Talk about taking control and contributing to scientific research.